Paying for care shouldn't be an issue.
We accept most insurance providers.
Zinnia Health is in-network with many leading insurance companies.
Select your insurance provider to check your coverage & verify your insurance.







Our Programs
Healing our heroes for good.

Prioritizing your mental health.







Who We Treat
What We Treat
Leading Clinical Outcomes
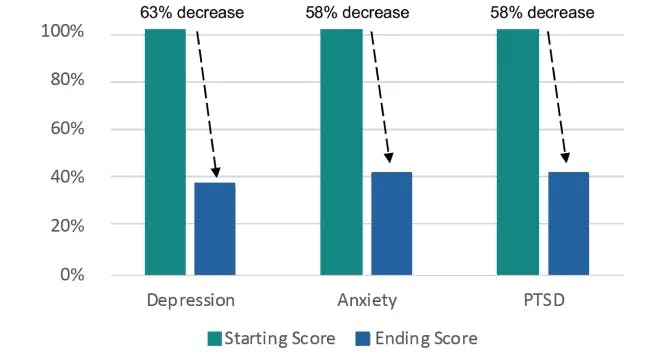
On average, clients who complete inpatient
care with Zinnia experience:
63% decrease in depression
moving into the minimal range
58% decrease in anxiety
moving into the minimal range
58% decrease in trauma/PTSD
moving out of the clinical range
Treatment options
that work for you.
Depending on which of our facilities you choose, we offer a variety of ways to help you tackle addiction and maintain a healthier lifestyle.
Detox
Our drug and alcohol detox centers have medical professionals, as well as 24-hour nursing staff, to help patients manage symptoms as comfortably as possible.
Inpatient Treatment
Some patients need a safe, supportive, and nurturing environment without any distractions to achieve success.
Partial Hospitalization Program (PHP)
This level of care offers a safe, structured outpatient environment to honestly confront your addiction and underlying issues.











